Standing pain rarely begins in the heel, even though that’s where it ends up. The chain reaction starts higher—in alignment, weight distribution, and muscle firing patterns that either protect the plantar fascia or overload it. For people who stand for hours, small posture failures repeat thousands of times a day, turning mechanical stress into injury patterns that linger.
The Impact of Proper Foot Alignment on Reducing Plantar Fasciitis Strain
Foot alignment determines how force travels from the ground to the heel and arch. The plantar fascia works like a tension bridge, stabilizing the arch, but it wasn’t designed to act as a shock absorber. If the foot collapses inward (overpronation) or rolls outward, that band of connective tissue stretches beyond its capacity, creating microtears that lead to chronic heel pain. What many don’t realize is that misalignment doesn’t have to look dramatic to cause damage. Even small deviations change the load path, forcing the arch to flatten under pressure. A plantar fasciitis specialist looks for these subtle positioning errors first, because correcting them early reduces strain before inflammation becomes persistent.
How Adjusting Your Standing Posture Can Relieve Foot Pain
Posture isn’t just about standing straight—it affects pressure points below the ankle. If the pelvis drifts forward, the calves tighten. If the shoulders fall back too far, the body compensates by shifting weight into the heels. Both scenarios increase pull on the plantar fascia during still standing.
Balanced posture allows muscles to share the workload instead of forcing the fascia to stabilize alone. Weight should center through the midfoot, not the heel cup or toes. Many patients who see a plantar fasciitis doctor improve noticeably when posture adjustments distribute force evenly rather than dumping it into one area for hours at a time.
Simple Posture Changes to Improve Plantar Fasciitis Symptoms
A small ergonomic shift can rewrite the entire loading pattern in the foot. Standing with knees softly unlocked keeps the gastrocnemius and Achilles from becoming rigid tension cables pulling at the heel. Keeping ribs stacked over hips prevents an exaggerated curve in the lower back that disrupts standing balance.
Neutral hip rotation matters more than most expect. If the toes point outward consistently, the arch twists downward under load. Bringing the feet forward and allowing the second toe, ankle, and knee to line up reduces rotational stress. These micro-corrections feel minor in the moment but change force repetition totals over an eight-hour shift.
The Role of Footwear in Preventing Strain During Prolonged Standing
Shoes determine how the foot interacts with the ground long before posture has a chance to correct anything. Hard, flat insoles increase fascia strain, while overly soft foam lets the arch collapse deeper into pronation. The best supportive designs absorb shock while preserving structure, creating a stable base rather than a cushioned sinkhole.
Heel-to-toe drop also affects tendon tension. Extremely flat shoes overstretch the plantar fascia, while excessively elevated heels shorten it, causing painful recoil when weight shifts forward. Footwear that supports alignment works as a preventative measure, but it is not a standalone fix for ongoing plantar fasciitis symptoms. Long-term pain patterns often require clinical insight to reverse the underlying mechanics.
Correcting Body Mechanics to Minimize Plantar Fasciitis Discomfort
The body defaults to the path of least resistance, even if that path increases strain. People with heel pain unknowingly shift weight to avoid discomfort, which creates overloading on the opposite side, shortening step patterns, tightening calves, or locking the knees during standing. These compensation habits become learned movement. Rewriting body mechanics requires sequencing—starting with ankle mobility, then knee tracking, hip symmetry, and pelvic neutrality. Patients examined by a plantar fasciitis specialist often find that heel pain decreases when the entire kinetic chain is coached into coordinated movement instead of treating the foot as an isolated problem.
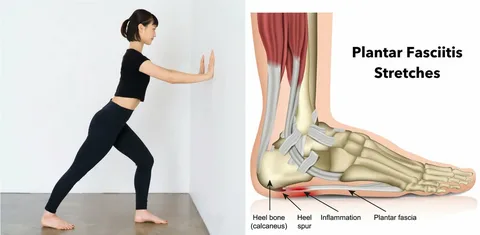
Stretching Techniques That Complement Posture Adjustments for Foot Health
Stretching without posture correction is like loosening one side of a knotted rope while the other side stays pulled tight. The goal isn’t just length, it’s balance. Lengthening the calf group reduces downward pull on the heel, while opening the hamstrings prevents posterior pelvic tilt that shifts standing pressure backward.
Effective stretching sequences are timed, not forced. Short controlled stretches done repeatedly retrain resting muscle tone faster than aggressive stretching that causes reflexive muscle guarding. Many people improve faster under supervised care, as technique precision determines whether stretches reduce strain or unintentionally intensify it.
How Maintaining Neutral Posture Can Alleviate Heel Pain
Neutral posture maintains the foot’s natural arch geometry instead of forcing plantar tissue to create artificial support through tension. In this position, the heel settles without jamming, the arch stabilizes without collapsing, and calf muscles lengthen without pulling like anchor ropes on heel bone attachment sites.
Fatigue is the real test. Proper alignment must hold when muscles get tired, which is why endurance training for postural stabilizers is often built into treatment plans. A plantar fasciitis doctor evaluates a patient’s ability to maintain neutral under load, because brief corrections don’t change symptoms unless the body can sustain the improved position over time.
Persistent heel pain that interferes with standing function deserves more than temporary workarounds, and clinical support can shorten recovery timelines—care teams at The Foot Clinic specialize in evaluating posture-driven strain patterns and long-term plantar fascia support strategies.